FAQ’s
Application
What can TMS be used for?
TMS is primarily utilized for the treatment of depression and anxiety. There is also benefit noted in the following conditions:
Psychiatric conditions:
Depression
Anxiety
Burnout
Substance abuse
Eating Disorders
Obsessive Compulsive Disorder (OCD)
Post-natal depression
Post-traumatic stress disorder (PTSD)
Neurological conditions:
Addiction (cocaine & food)
Chronic pain
Fibromyalgia
Migraine
Questions answered
Frequently Asked Questions
TMS is an effective process in which a focused magnetic field stimulates under-active brain cells, activates them to work more efficiently and transforms lives through symptom reduction.
TMS is particularly effective when used to treat depression, anxiety and burnout that has not fully responded to conventional treatments (medication/therapy).
No. TMS is primarily recommended for treatment resistant illness and in that context, is intended to be an adjunctive (additional) treatment. That being said, given repose rates and tolerability, increasingly clients are opting for TMS earlier in the course of their illness prior to trying medication. While receiving TMS, we would ask that no medication changes be undertaken if at all possible. For those that thereafter achieve either complete remission or significant improvement, it is important that any changes to medication proceed under the supervision of your usual treating team.
TMS
- Hospital admission not required (out-patient)
- Non invasive
- indirect application of magnetic pulse
- Awake & alert throughout
- No recovery time needed after treatment (the patient can drive and return to work immediately)
- Side effects – mild and uncommon.
- Seizure occurrence is rare, with no impact on memory function
- Research suggests potentially as effective as ECT
ECT
- Usually performed in hospital (admission required)
- Non invasive
- Direct application of low amplitude electrical current
- General anaesthesia required (carries a rare mortality risk)
- Period of recovery time and nursing observation required after treatment
- Seizure induced (integral to mechanism of action) & can cause long-term damage to memory
- Historical gold standard treatment of depression
An individual may be suitable for TMS if he or she:
- has a diagnosis of depression (especially treatment resistant depression)
- has had difficulty coping with some of the side effects of medication
- does not wish to take medication
- does not wish to undergo Electroconvulsive Therapy (ECT)
- suffers with any of the other disorders listed earlier (see section what is TMS used for?)
As a general rule, TMS works best when it is given relatively early in the course of the illness, and results are better if the treatment course is completed. Our experience shows it works remarkably well, even for clients with a high level of treatment resistance. Given its mechanism of action, TMS cannot proceed if the person is pregnant, has a personal or family history of seizure (or other neurological) disorder, has active alcohol or drug dependency, has ANY metal fragments in the brain, eye, ear or heart or is younger than 16 years of age.
The average number of treatment sessions is 30 over a period of two weeks.
This ultimately depends on the individual. Patients commonly report sustained improvement several months following treatment. For some in whom depressive symptoms recur, an individualised maintenance program can maintain recovery without having to repeat the initial induction course.
Once assessed and the appropriate treatment protocol is determined, the treatment session typically lasts less than 5 minutes. This is achieved using a revolutionary software upgrade to the treatment called ‘Theta Burst Stimulation (TBS) which allows us to administer three rapid treatment sessions in a single 15 minute appointment. As a consequence, the total treatment course can be completed from Mon-Friday over ten working days. Clients are at all times sitting comfortably and alert. For this reason we encourage individuals to engage with therapy whilst receiving their treatment. During treatment the magnetic coil is suspended over the appropriate region of the person’s scalp. The client perceives a series of clicking noises followed by a pause as the magnet rapidly turns on and off gently pulsating activating energy to the desired brain region. Following treatment, the client can immediately resume daily activities.
Treatment resistant depression (TRD) is depression that has failed to respond in any meaningful way to conventional treatment (medication/psychological therapy). Depression itself is a complex illness that can diminish a person’s enjoyment or engagement with his/her loved ones, friends, education or career. In addition to the psychological feelings of despair and guilt, it can have a physical basis and adversely affect one’s sleep pattern, energy levels and sex drive, as well as other symptoms such as muscle pain. For some, coping with this illness can become difficult and they can become hopeless, even suicidal. For these reasons, the World Health Organisation recognises depression as the illness with the greatest morbidity. TMS is helping to turn treatment resistance into recovery attainment.
Yes! It is approved by Health Canada (2005), Food and Drug Administration (FDA), United States (2008) and the National Institute for Health and Clinical Excellence (NICE), United Kingdom (2015).
The core scientific principles of TMS (electromagnetic induction) are well established. Research into its physiological/clinical applications began in the 1980s leading to its approval by Health Canada (2005), as a safe and effective treatment for depression. Since it received FDA approval in the United States, TMS is now covered by insurance policies in 41 of 50 states. TMS is now covered by insurance in all 50 States in the United Sates’. In Canada some insurance companies consider part payment of the treatment on a case by case basis.
question
What is Burnout?
The World Health Organisation (WHO) International Classification of Disease 11th Edition defines Burnout as:
“..a syndrome conceptualised as resulting from chronic workplace stress that has not been successfully managed. It is characterised by three dimensions:
– feelings of energy depletion or exhaustion;
– increased mental distance from one’s job, or feelings
of negativism or cynicism related to one’s job; and
– reduced professional efficacy.
It is facilitated by a culture that demonstrates
• Unfair treatment of the employees
• Unmanageable wok loads for employees
• Unclear communication from managers
• Lack of manager support
• Unreasonable time pressures on employees.
Why is Burnout Important?
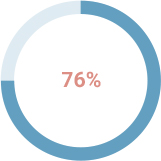
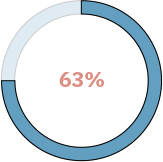
of employees experience burnout on the job at least sometimes
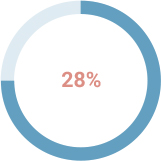
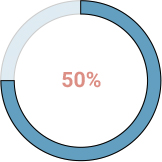
of employees experience burnout “very often”or “always”
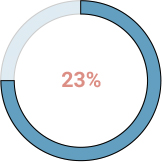
of employees with burnout are more likely to take a sick day
of employees with burnout are less likely to discuss how to approach performance goals with their manager
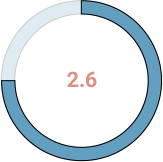
more likely to visit the emergency room for physical ill-health
times more likely to be actively seeking a different job